You are here
Zika Contraceptive Access Network Provides a Roadmap for Success
In 2014, few people outside of infectious disease experts had ever even heard of the Zika virus, a mosquito-borne disease like malaria and West Nile virus. However, in 2015 and 2016, Zika quickly became a public health emergency as large outbreaks of the virus occurred across the southern United States and U.S. territories. In one year, reported cases of Zika in Puerto Rico and the U.S. Virgin Islands exploded from just nine in 2015 to almost 37,000 by the end of 2016. A staggering 86 percent of all cases reported in the U.S. and its territories occurred in Puerto Rico.
Unlike other mosquito-borne diseases, Zika is also sexually transmitted and can pass from a pregnant woman to her unborn child. Although Zika is mild in adults, five percent of children infected with Zika in-utero are born with serious birth defects, like microcephaly.
Women in Puerto Rico faced limited availability of contraceptives, high out-of-pocket costs and a shortage of trained physicians. In 2016, two-thirds of pregnancies in Puerto Rico were unintended. During the outbreak, the number of pregnant women infected with Zika increased from 8 percent in February 2016 to 41 percent in June 2016. Because of this enormous risk, contraceptives were used as a medical countermeasure to allow women to delay pregnancy until the outbreak ended.
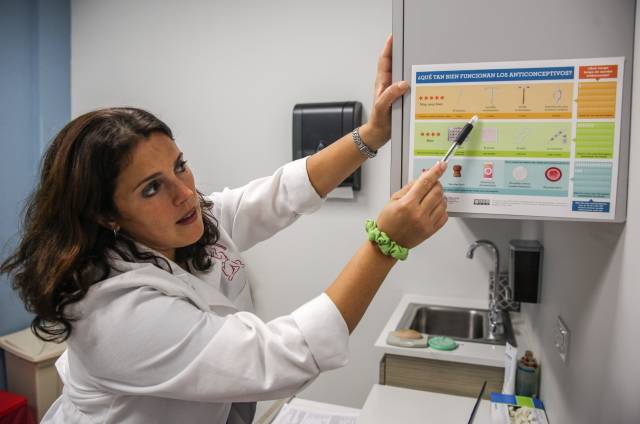
In response, the CDC Foundation, in partnership with a diverse group of public and private partners, and with technical assistance from CDC, established the Zika Contraception Access Network (Z-CAN). This short-term intervention provided free, full-range, reversible contraceptive services for women in Puerto Rico by building capacity among healthcare providers, procuring and distributing contraceptive methods and supporting overall clinic needs.
The Z-CAN program saw immediate success. From 2016 to 2017, Z-CAN served more than 29,000 women, 70 percent of whom chose previously inaccessible long-acting reversible contraceptive (LARC) methods, which included intrauterine devices (IUDs) and implants. Eighty five percent of patients reported high levels of satisfaction with the contraceptive services, and notably, three years later, most patients were still using their LARC.
In consideration of Puerto Rico’s history of unethical sterilization and birth control testing, safeguards were put in place to ensure women receiving Z-CAN contraceptive services had full control at every step and were able to choose birth control that best met their reproductive needs. Through Z-CAN’s safety net program, women also had guaranteed access to no-cost removal of their contraceptive devices for up to 10 years after the program ended.
“The Z-CAN program managed to change the perspective on contraceptive methods and family planning in Puerto Rico,” said Marilyn Colon Lopez, field employee at the CDC Foundation, who maintains the safety net’s communication channels. “Puerto Rican women were oriented with the diversity of methods through our program, and they never felt alone in the process. Thousands were served and managed to get the methods completely free.”
During the outbreak, which ended in 2017, Z-CAN is estimated to have prevented 85 percent of Zika-associated microcephaly and nearly 10,000 unintended pregnancies. At a final implementation cost of $26.1 million, Z-CAN saved $79.9 million in Zika-associated costs and $137 million in costs related to unintended pregnancy.
Though the program ended in 2017, the safety net will remain active until 2027. “This critical element of the program ensures women who participate have full autonomy and access to the reproductive care they need in the long term,” said Rachel Powell Lewis, PhD, MPH, senior program manager at the CDC Foundation.
Z-CAN demonstrated the vital role of public-private partnerships and the importance of ethical safeguards. The project also showed that an emergency response to a public health crisis can be implemented both quickly and cost-effectively. The program and ongoing safety net have also provided the CDC Foundation with an invaluable roadmap for future intervention planning. Part of the program’s legacy has been to share that roadmap, the Increasing Access to Contraception Toolkit, with public health professionals interested in learning about, replicating or adapting elements of the Z-CAN program. These lessons provide the global health and US-based community with the tools we need to prepare and respond to the next public health emergency.
Photo credit: Evelyn Hockstein/CDC Foundation