Revitalizing Zambia’s Vital Statistics: Strengthening Cause-of-Death Data to Save Lives
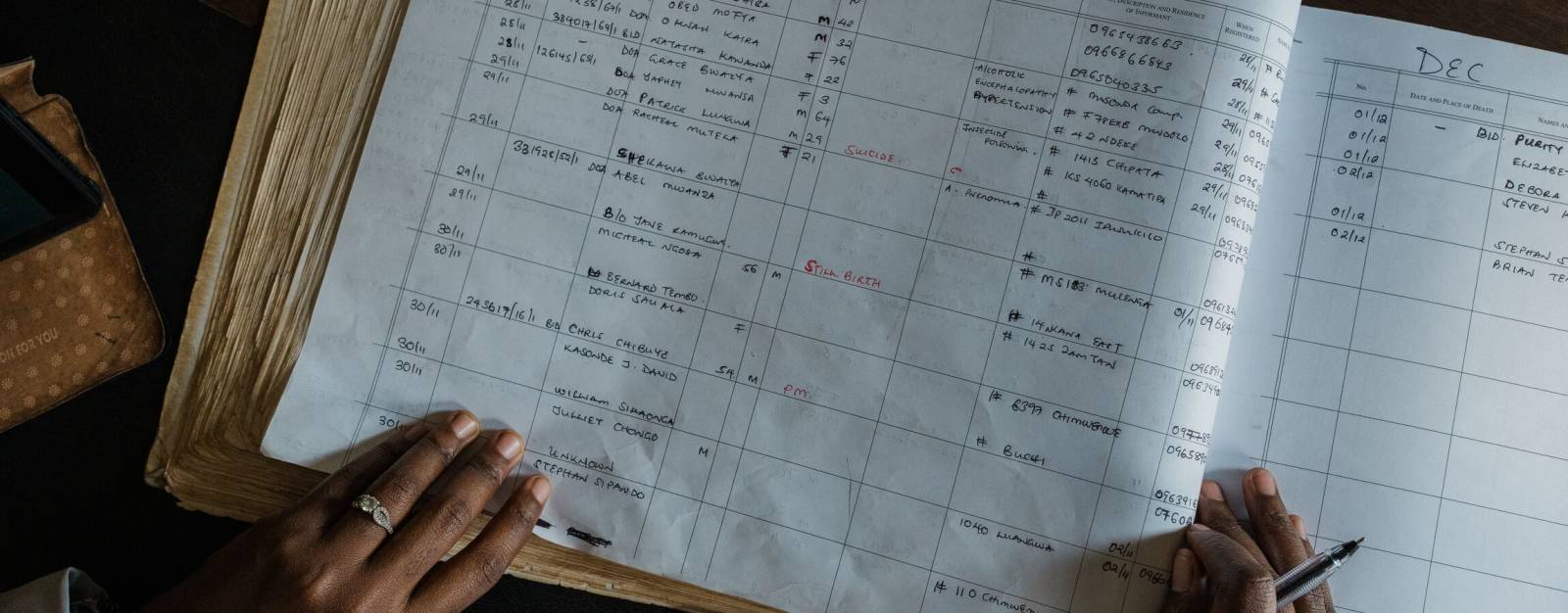
It remains difficult for many countries around the globe to collect and maintain cause of death (COD) data that’s up-to-date, accurate and available to decision-makers. Before 2015, Zambia—a sub-Saharan African country that’s home to about 20 million people—faced a critical gap in COD data from its civil registration and vital statistics (CRVS) system. With less than four percent of deaths officially registered, public health officials lacked a meaningful understanding of why fatalities were occurring, leaving communities and health systems without a coordinated response to noncommunicable diseases and unprepared for health threats.
An effective public health system relies on a strong CRVS system that accurately records births and deaths, including causes of death, so resources can be effectively allocated and critical health challenges addressed. Zambia's CRVS system was hindered by fragmented reporting processes and limited expertise in certifying and coding COD data. Doctors often struggled to accurately complete medical certification of cause of death (MCCD) forms, and deaths occurring outside of hospitals were largely undocumented.
In 2015, the CDC Foundation started working with the Bloomberg Philanthropies Data for Health Initiative in Zambia, partnering with several Zambian government agencies and national organizations: the Department of National Registration, Passport and Citizenship (DNRPC), Ministry of Health, Zambia Medical Association (ZMA) and Zambia Statistics Agency (ZamStats). Partners also included international organizations such as UNICEF, the World Health Organization (WHO) and the U.S. Centers for Disease Control and Prevention (CDC). The goal was to strengthen Zambia’s CRVS system and improve COD data for informed public health decision-making.
Laying the Foundation: Governance and Coordination
The effort began by bringing together a CRVS technical working group comprised of partners from various sectors, including government ministries, public safety and local government entities. Using flowcharts to visually represent the steps in their processes, a methodology called business process mapping, the team identified stakeholder roles, bottlenecks in the CRVS system and shared goals. This collaborative approach led to a national strategic plan for CRVS improvement, laying the groundwork for transformative change.
Training in MCCD and Coding
Training became a cornerstone of the initiative. In 2016, the first MCCD sessions for “training of trainers” were held, followed by training an initial cohort of doctors at Lusaka’s main hospital, and then expanding to other health facilities and districts. The MCCD course, based on global guidelines, was integrated into Zambia Medical Association’s continuing medical education program, which is required for doctors to renew their licenses. An e-learning platform linked to the Health Professions Council of Zambia further facilitated access. By 2024, more than 5,000 practicing doctors had received this training. MCCD instruction was also embedded in medical school curricula, ensuring that future generations of healthcare providers would be equipped to certify COD data accurately.
Another key achievement was the establishment of a mortality coding center in 2016. This center, initially developed for a previous global health project, was repurposed and enhanced to process updated MCCD forms from health facility deaths. Full-time staff were trained to code the forms using the International Classification of Diseases (ICD) to ensure consistency and comparability of data across different regions and time periods. The Zambian government’s inclusion of mortality coding functionalities into the CRVS system and absorbing of the coding staff ensured the center’s sustainability. With better data entering the system, the Zambia Statistical Agency published its first National Vital Statistics Report in 2019, a milestone for the country.
Dr. Luchenga Adam Mucheleng’anga, Zambia’s leading forensic pathologist, conducts a morning briefing with his doctors, including fellow forensic pathologists and support staff, at the University Teaching Hospital in Lusaka, Zambia.
Addressing Non-Facility Deaths with Verbal Autopsies
To capture more data on deaths occurring outside health facilities—about 47 percent of all deaths in Zambia—verbal autopsies (VA) were introduced at select sites in 2017. VA involves sending trained interviewers to determine the likely cause of death with information from the deceased’s family members or caregivers. These interviews, based on the globally standardized VA questionnaire, were initially conducted at mortuary sites and then expanded to interviewing family members in the community. Verbal autopsies have proven invaluable during public health crises in Zambia, such as the COVID-19 pandemic and cholera outbreaks, and in understanding the prevalence of noncommunicable diseases. VAs have also strengthened HIV surveillance, leading to understanding of HIV-related mortality by identifying HIV-associated deaths in the absence of medical records. Today, VA is operational at 35 sites, which cover nearly half of Zambia’s population.
Medico-Legal Death Investigations
The enactment of the National Forensic Act No. 2 of 2020 institutionalized the Medico-Legal Death Investigation (MLDI) system in Zambia, providing a regulatory framework for forensic science and pathology. This system has improved the coordination of forensic investigations and the accuracy of COD reporting for non-facility deaths, further enhancing public health data.
The Impact: Informed Public Health Decisions
These efforts by the Zambian government and project team have significantly improved Zambia’s COD data. By 2023, the proportion of registered deaths increased from four percent to 42 percent, while the percentage of ill-defined causes of death dropped from 40 percent to less than 26 percent. Families now receive death certificates with accurate COD information, fostering transparency and closure. High-quality data also enables evidence-based policymaking and better allocation of resources. The strengthened CRVS system has become a critical asset for the Zambia National Public Health Institute’s Mortality Surveillance Unit, supporting targeted public health responses.
Looking Ahead
Plans are underway to digitalize the paper-based CRVS system, as well as expand VA and mortality coding to underserved areas and refine data analysis for more targeted health interventions. Zambia’s achievements now serve as a model for other low- and middle-income countries seeking to enhance the use of CRVS data for public health policy—underscoring the power of data to save lives and shape a healthier future.
Promising Practices
The following strategies may be helpful to other countries aiming to strengthen their CRVS system and COD data.
- Engage stakeholders from national ministries, local governments and communities and other sectors to identify issues and shared goals and create a coordinated improvement plan.
- Conduct extensive training for healthcare professionals on accepted Medical Certification of Cause of Death (MCCD) guidelines. Integrating this training into continuing medical education requirements and medical school curricula can enable buy-in and long-term sustainability. An e-learning platform will also facilitate widespread access to training.
- Use verbal autopsies for non-facility deaths to address data gaps and provide critical insights, including during health crises. Enacting regulatory frameworks, like Zambia’s National Forensic Act, will help formalize and improve forensic coordination and COD reporting for non-facility deaths.
- Help ensure sustainability through government commitment to funding critical infrastructure and operations, like coders’ salaries and CRVS system management.
- Use business process mapping to identify systemic weaknesses and design targeted, effective solutions.
- Start small at pilot sites to expand successful interventions across regions.
Photos: Juan Arredondo